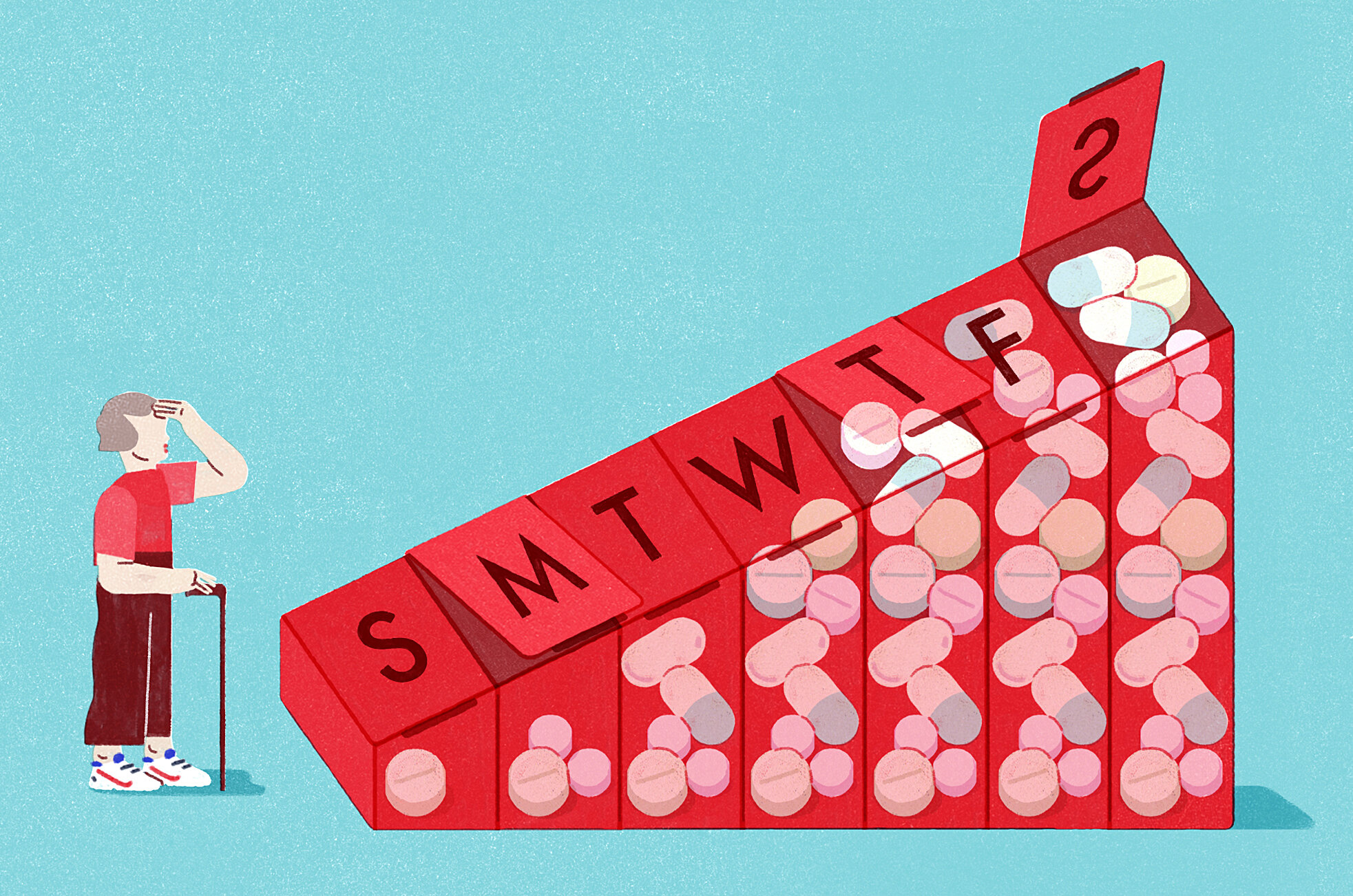
After reading both texts, the fact about medication and older adults that surprised me the most was the amount of medication being prescribed to the patients despite knowing or ignoring the harm that is and/or can be caused by it or as Aronson (2019) calls it, “prescribing cascade.” According to Cruikshank, “each year, 100,000 Americans or more die of adverse drug reactions, one million severely injured, and two million are harmed while they are hospitalized. And approximately 17 percent of hospital admission of people over 70 are caused by adverse reaction to drug mostly caused by overmedication” (Cruikshank, 2013, p.4). The saying “Primum non nocere (First, do no harm)” immediately came to mind which is why I was surprised by how common this was amongst elderly patients. With such a fragile population, I would assume that they would be among the most protected in healthcare.
It is inevitable that our body will go through changes as we age such as the slowing down of our metabolism, weight change, and loss of body mass. Many, especially old women, are denied the experience of aging-whatever it might be for them- because the chemicals in their bodies are literally changing who they are. And their doctors have unwittingly taken control of their aging (Cruikshank, 2013). Having to depend on others and losing decision-making abilities is another fear of mine when it comes to growing older. Because drug reactions disproportionally affect women than men, drug-free aging as suggested by Cruikshank is the goal and this can be done by making better life choices such as exercising, changing my diet and seeking alternative treatment.
The conversation between Aronson and Svetlana was a prime example of how having a conversation and taking the time out to listen and learn about your patients can literally be life or death. According to Aronson, “In a health care system where time is the scarcest resource and care is fragmented among doctors without clear mechanism for designating a recognized team captain, new symptoms are too often attributed to age and disease rather than to the care or drugs that actually caused them” (Aronson, 2019, p.48). After their conversation and doing some digging, it was determined that Dimitri’s deterioration was drug-induced.
One interesting fact that Aronson stated that I was intrigued by was the fact that only certain doctors learned about Dementia until recently and how different their learning was/is. According to Aronson, 2019, “Neurologist prioritized diagnosis by brain pathology and treatment with medication. Psychiatrists attended to dementia patients’ anxiety, depression and psychotic symptoms. And geriatricians, focused on managing a patient’s health social situation, and physical environment to maximize their and their caregivers’ well-being” (Aronson, 2019, p.53). Similar to the Memory Loss Tapes, Aronson reminded me that Dementia is deeper than science and forces us to deal with the true reality of human behavior that most researchers fail to mention.
Lastly, I found it interesting that Gabow chose an alternative approach to treating her mother instead of moving forward with surgery as she would have normally done for her patients. What had the biggest impact on me was Gabow’s realization that her standards did not address the needs of all patient populations because every patient is unique and what works for one may not work for most.
Aronson, L. (2019). Elderhood: Redefining aging, transforming medicine, reimagining life. Bloomsbury Publishing.
Cruikshank, M. (2013). Learning to be old: Gender, culture, and aging (3rd ed.). Rowman & Littlefield.
0 Comments